
Hot potato causing full-thickness esophageal burn and perforation: a case report
Highlight box
Key findings
• This report describes a full-thickness esophageal burn and perforation after the ingestion of a microwave-heated new potato.
What is known and what is new?
• Acute thermal injuries to the esophagus are uncommon causes of esophageal injury.
• Various degrees of esophageal injury have been reported depending on the temperature, amount of ingested food, physical state, and exposure time.
• We describe the first case of esophageal burn and full-thickness perforation after the ingestion of a microwave-heated new potato.
What is the implication, and what should change now?
• Despite this being anecdotal evidence, ingestion and impaction of microwave-heated solid food may potentially cause full-thickness esophageal perforation thus representing an esophageal emergency.
Introduction
The majority (60%) of esophageal perforations are iatrogenic and occur during diagnostic and therapeutic endoscopic procedures (1). Spontaneous, foreign bodies, and trauma are responsible for 15%, 8%, and 5% of esophageal full-thickness perforation, respectively (2-4). The common denominator of these heterogeneous conditions is mediastinal contamination by digestive contents and the evolution to severe sepsis and death in the absence of timely diagnosis and appropriate treatment (5,6). Mortality ranges between 10% and 20% and the delay in treatment is the most important survival predictor (7-9).
We describe the case of a swallowed microwave-heated potato causing esophageal thermal injury and punched-out perforation of the thoracic esophagus. We present this article in accordance with the CARE reporting checklist (available at https://aoe.amegroups.org/article/view/10.21037/aoe-23-17/rc).
Case Presentation
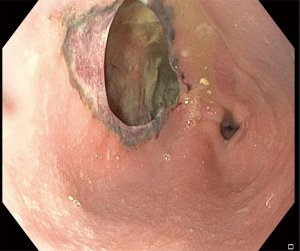
A 38-year-old man without apparent psychiatric/neurologic comorbidities was referred to our hospital 36 hours after the acute onset of dysphagia, drooling and worsening thoracic pain after ingestion of a microwave-heated novel potato. The chest X-ray showed evidence of pneumomediastinum. A chest computed tomography (CT) confirmed the presence of pneumomediastinum, left hydropneumothorax and soluble contrast extravasation (Figure 1). The upper endoscopy showed a 4 cm × 2 cm esophageal full-thickness parietal loss located at 30 cm from the incisors. The mucosal edges of the perforation were scarred and inflamed as occurs in thermal injuries (Figure 2 and Video 1). On arrival, the patient was febrile (38.6 ℃), tachycardic (116 bpm), and tachypneic, with normal blood pressure (130/85 mmHg). The physical examination did not reveal subcutaneous emphysema. White blood cell count (18,500/mm3), C-reactive protein (38 mg/dL), procalcitonin (2.35 ng/mL), and lactate (1.98 mmol/L) were altered. The patient underwent hybrid esophagectomy via laparoscopy and right thoracotomy with gastric conduit reconstruction. A circular stapled 25 mm anastomosis was fashioned at the apex of the thorax and a pleural patch was used to reinforce the suture. Both the right and left chest were drained and a feeding jejunostomy was performed for nutritional support. The postoperative course was uneventful. An upper endoscopy performed on postoperative day (POD) 5 showed regular anastomosis. The patient was discharged home on POD 9 on a soft diet. The histological examination of the specimen did not reveal peculiar alterations. At 8-month follow-up, the patient was doing well with a well-tolerated regular diet. The upper endoscopy showed normal anastomosis and gastric conduit. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the institutional ethics board of IRCCS Ospedale Galeazzi - Sant’Ambrogio (No. #2023-OGSA1452).

Discussion
Esophageal perforations are transmural disruptions of the esophageal wall leading to leakage of intraluminal contents into the surrounding mediastinum and pleural cavities. This causes local inflammation with the development of systemic inflammatory response and sepsis, and high risk of mortality (1). Non-operative management (NOM) and endoscopic treatment can be considered in stable patients with early presentation, limited esophageal disruption, and contained contamination (8-10). On the contrary, surgery should be considered in patients who do not meet NOM criteria. General principles of surgical management include exposure, debridement of non-viable tissue, tension-free defect closure, suture buttressing, and drainage. Esophageal exclusion, diversion, or resection should be considered when primary repair is not feasible.
Acute thermal injuries to the esophagus are uncommon causes of esophageal injury (11). Various degrees of esophageal injury have been reported depending on the temperature, amount of ingested food, physical state (i.e., liquid or solid), and exposure time (12). Linear erythema with white pseudomembranes has been described after ingestion of hot beverages (candy-cane esophagus) (11). These injuries are usually superficial and self-limiting. Similarly, hot solid foods may cause mucosal thermal injury (12,13). The damage pattern is heterogeneous with superficial ulceration, linear erythema, and submucosal blister while no perforations have been described until now. To the best of our knowledge, this is the first reported case of full-thickness esophageal perforation after ingestion of a microwave-heated new potato. New potatoes are not a specific variety; any potato that is harvested early in the season is called new. Other than the small size, a characteristic of new potato is that they keep their shape and consistency once oven or microwave cooked. Differently from the conventional oven heating that involves heat transfer from outside to inside, microwave heating involves energy conversion from electromagnetic to thermal energy. Microwaves are low-energy electromagnetic waves with a wavelength in the range of 0.001–0.3 meters and a frequency in the range of 1,000–300,000 MHz. During the heating process, electromagnetic waves oscillate within the oven and interact with food particles, leading to heat generation and rise in temperature. Specifically, microwaves cause heating from the inner layers toward the outer layers. This generates an inside-out thermic effect while internal parts are heated faster than those located outside. In the present case, we can assume that the ingested potato was warm outside and hot in the core. The single-swallow ingestion of this potato impacted the thoracic esophagus causing acute onset of dysphagia and drooling. The mechanism of damage may be attributable to the protracted thermal injury with consequent punched-out full-thickness delayed perforation. Because of the significant wall defect with loss of tissue (Figure 2) in conjunction with endoscopic evidence of burned and scarred edges, primary repair was not attempted whereas esophagectomy was preferred (14). Thoracotomy was preferred over a minimally invasive approach to obtain a better exposure of the middle third of the esophagus and faster infectious source control. Because of the limited right pleural space contamination, the anastomosis was located at the apex of the thorax and reinforced with a mediastinal pleural patch to possibly reduce the risk of leak (15,16).
Conclusions
Despite this being anecdotal evidence, ingestion and impaction of microwave-heated solid food may potentially cause full-thickness esophageal perforation.
Acknowledgments
Funding: The article has been supported by AIRES (Associazione Italiana Ricerca ESofago).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aoe.amegroups.org/article/view/10.21037/aoe-23-17/rc
Peer Review File: Available at https://aoe.amegroups.org/article/view/10.21037/aoe-23-17/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoe.amegroups.org/article/view/10.21037/aoe-23-17/coif). L.B. serves as an unpaid editorial board member of Annals of Esophagus from October 2023 to September 2025. The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the institutional ethics board of IRCCS Ospedale Galeazzi - Sant’Ambrogio (No. #2023-OGSA1452).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chirica M, Kelly MD, Siboni S, et al. Esophageal emergencies: WSES guidelines. World J Emerg Surg 2019;14:26. [Crossref] [PubMed]
- Aiolfi A, Micheletto G, Guerrazzi G, et al. Minimally invasive surgical management of Boerhaave's syndrome: a narrative literature review. J Thorac Dis 2020;12:4411-7. [Crossref] [PubMed]
- Aiolfi A, Ferrari D, Riva CG, et al. Esophageal foreign bodies in adults: systematic review of the literature. Scand J Gastroenterol 2018;53:1171-8. [Crossref] [PubMed]
- Aiolfi A, Inaba K, Recinos G, et al. Non-iatrogenic esophageal injury: a retrospective analysis from the National Trauma Data Bank. World J Emerg Surg 2017;12:19. [Crossref] [PubMed]
- Ali JT, Rice RD, David EA, et al. Perforated esophageal intervention focus (PERF) study: a multi-center examination of contemporary treatment. Dis Esophagus 2017;30:1-8. [Crossref] [PubMed]
- Vermeulen BD, van der Leeden B, Ali JT, et al. Early diagnosis is associated with improved clinical outcomes in benign esophageal perforation: an individual patient data meta-analysis. Surg Endosc 2021;35:3492-505. [Crossref] [PubMed]
- Biancari F, D'Andrea V, Paone R, et al. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 2013;37:1051-9. [Crossref] [PubMed]
- Abbas G, Schuchert MJ, Pettiford BL, et al. Contemporaneous management of esophageal perforation. Surgery 2009;146:749-55; discussion 755-6. [Crossref] [PubMed]
- Schweigert M, Sousa HS, Solymosi N, et al. Spotlight on esophageal perforation: A multinational study using the Pittsburgh esophageal perforation severity scoring system. J Thorac Cardiovasc Surg 2016;151:1002-9. [Crossref] [PubMed]
- Bona D, Aiolfi A, Rausa E, et al. Management of Boerhaave's syndrome with an over-the-scope clip. Eur J Cardiothorac Surg 2014;45:752-4. [Crossref] [PubMed]
- Dutta SK, Chung KY, Bhagavan BS. Thermal injury of the esophagus. N Engl J Med 1998;339:480-1. [Crossref] [PubMed]
- Lee YM, Kim SM, Kim JY, et al. Various upper endoscopic findings of acute esophageal thermal injury induced by diverse food: a case series. Clin Endosc 2014;47:447-51. [Crossref] [PubMed]
- Chung WC, Paik CN, Jung JH, et al. Acute thermal injury of the esophagus from solid food: clinical course and endoscopic findings. J Korean Med Sci 2010;25:489-91. [Crossref] [PubMed]
- Bonavina L, Asti E, Sironi A, et al. Hybrid and total minimally invasive esophagectomy: how I do it. J Thorac Dis 2017;9:S761-72. [Crossref] [PubMed]
- Asteriou C, Barbetakis N, Lalountas M, et al. Modified pleural tenting for prevention of anastomotic leak after Ivor Lewis esophagogastrectomy. Ann Surg Oncol 2011;18:3737-42. [Crossref] [PubMed]
- Axtell AL, Gaissert HA, Morse CR, et al. Management and outcomes of esophageal perforation. Dis Esophagus 2022;35:doab039. [Crossref] [PubMed]
Cite this article as: Aiolfi A, Manara M, Bargiggia S, Fardowza N, Cirri S, Bonavina L, Bona D. Hot potato causing full-thickness esophageal burn and perforation: a case report. Ann Esophagus 2024;7:7.


