
Comparison of the Comprehensive Complication Index and Clavien-Dindo Classification for grading of postoperative complications after Ivor-Lewis esophagectomy in a high-volume center
Introduction
The quality of medical treatment can be measured by different means, e.g., survival, R-status, recurrence of disease, Length of hospital stay (LOS) but also by the complications caused by the treatment itself.
In 1992, Clavien et al. proposed a complication scoring system categorizing complications depending on the treatment they require (1). After revision in 2004, it is known as the Clavien-Dindo Classification (CDC) ever since. It has widely been used and was proven to correctly measure outcome after complications in surgery (2-4). It categorizes complications into 7 different ranks (I, II, IIIa/b, IVa/b, V) (Table 1). Only the highest rated complication is then being used to describe the surgical outcome in terms of complications (1,2). Hiroshi Katayama and the Japan Clinical Oncology Group proposed extended evaluation criteria of certain postoperative complications, thus helping to develop a universally more standardized evaluation of complications (5).
Table 1
| CDC grade | Treatment required/definition |
|---|---|
| I | Any deviation from the normal postoperative course, no treatment needed other than: analgesics, diuretics, antipyretics, physiotherapy, opening of wound at bed side |
| II | Pharmacological treatment required, e.g., blood transfusion, parenteral nutrition |
| III | Surgical, endoscopic or radiological intervention required |
| IIIa | No general anesthesia required |
| IIIb | General anesthesia required |
| IV | Life threatening complication/ICU required |
| IVa | Single organ failure |
| IVb | Multi organ failure |
| V | Death of patient |
CDC, Clavien-Dindo Classification; ICU, intensive care unit.
The obvious disadvantage of the CDC is that many patients experience more than one complication and therefore, the CDC is considered to underestimate the overall burden of postoperative complications.
To take into account all postoperative complications during one postoperative course, the Comprehensive Complication Index (CCI) was developed (3). It is based on the complication grading by CDC and implements every occurred complication after an intervention. It is calculated as the sum of all complications that are weighted for their severity. Overall morbidity is represented on a scale from 0 (no complication) to 100 (death).
So far, the CCI has been shown to better correlate with LOS as well as length of intensive care in general surgery (6,7) as well as complex procedures like gastrectomy (8), or surgery in inflammatory bowel disease (9).
Esophagectomy is regarded as high-risk surgery and is associated with high rates of complications (10,11). We therefore addressed the question if CCI better correlates with LOS than CDC after radical esophagectomy. We present this article in accordance with the STROBE reporting checklist (available at https://aoe.amegroups.com/article/view/10.21037/aoe-22-13/rc).
Methods
We performed a retrospective analysis involving all patients who underwent resection of the esophagus for cancer at our high-volume center for esophageal surgery in Offenbach from 2014 to 2018. Standard procedure was hybrid Ivor-Lewis esophagectomy with two field lymphadenectomies (laparoscopic abdominal surgery and open thoracic anastomosis). Patients were allowed clear liquids immediately after surgery. Solid oral intake was started on postoperative day 5 after a routine radiographic control of the anastomosis. Patient health records were individually screened for any kind of complication during the hospital stay and graded by an experienced surgeon using the CDC. CCI was derived from these scores, using the CCI calculator available online (www.assessurgery.com).
No IRB approval statement or ethics vote was obtained as the study was purely retrospective, data was anonymously used for the study and no harm whatsoever may be caused by inclusion in the study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Individual consent for this retrospective analysis was waived.
Statistical analysis
Standard statistical analyses were used for normally distributed metric variables. For binary variables, Chi square tests and U-tests were used.
Correlation of CCI with LOS was determined using Pearson correlation and correlation of CDC with LOS was determined using Spearman’s Rho correlation. The difference between CCI and CDC systems was controlled by comparison of 1 complication versus >1 complications using analysis of variance (ANOVA).
Confounder analysis with demographic, clinical and pathological covariates were performed. Significant variables were checked in a multivariate regression model for independent correlation with LOS.
All statistical tests were two-sided and P value of <0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 23.0 (IBM Corporation, New York, USA) and GraphPad Software (San Diego, CA, USA).
Results
During 04/2014 to 12/2018, 279 patients underwent Ivor-Lewis esophagectomy. Patient characteristics are shown in Table 2.
Table 2
| Variables | Numbers (n=279) |
|---|---|
| Age (years) | 63.5±9.6 [34–84] |
| ≤65 | 159 (57.0) |
| >65 | 120 (43.0) |
| Sex | |
| Male | 226 (81.0) |
| Female | 53 (19.0) |
| BMI (kg/m²) | 27±4.7 [18–52] |
| ASA | |
| I | 6 (2.2) |
| II | 169 (60.6) |
| III | 103 (36.9) |
| IV | 1 (0.4) |
| Local tumor stadium | |
| 0–1 | 150 (53.8) |
| 2 | 44 (15.8) |
| 3 | 85 (30.5) |
| Neoadjuvant treatment | |
| None | 127 (45.5) |
| Chemotherapy | 123 (44.1) |
| Radio-chemo therapy | 29 (10.4) |
| Histological subtype | |
| Adenocarcinoma | 249 (89.2) |
| Squamous cell carcinoma | 30 (10.8) |
| Type of surgery | |
| Hybrid (Ivor-Lewis) | 232 (83.2) |
| Open | 47 (16.8) |
| Duration of surgery (minutes) | 290±58 [164–574] |
| Extended surgery | 52 (18.2) |
| Cholecystectomy | 29 (10.4) |
| Lung resection | 14 (5) |
| Splenectomy | 2 (0.7) |
| Partial pancreatectomy | 2 (0.7) |
| Liver resection | 7 (2.5) |
| Postoperative ICU stay (days) | 7.2±5.1 [1–51] |
| Length of hospital stay (days) | 20.6±11 [7–90] |
Data are presented as mean ± SD [range] or n (%). n, number; SD, standard deviation; BMI, body mass index; ASA, American Society of Anaesthesiologists; ICU, intensive care unit.
Overall, we detected 277 complications in 162 patients; 95 patients had a single complication, 67 patients had more than one complication; 117 did not have any complications (Table 3).
Table 3
| Complications after esophagectomy | Numbers |
|---|---|
| CDC | |
| 0 | 117 (41.9) |
| I | 26 (9.3) |
| II | 79 (28.3) |
| IIIa | 22 (7.9) |
| IIIb | 16 (5.7) |
| IVa | 10 (3.6) |
| IVb | 6 (2.2) |
| V | 3 (1.1) |
| Number of complications per patient | |
| 1 | 95 (58.6) |
| 2 | 38 (23.5) |
| 3 | 17 (10.5) |
| 4 | 6 (3.7) |
| 5 | 5 (3.1) |
| 6 | 1 (0.6) |
| Overall CCI (n=279) | 16.6±19.5 [0–100] |
| CCI >0 (n=162) | 28.6±17.6 [8.7–100] |
Data are presented as mean ± SD [range] or n (%). CDC, Clavien-Dindo Classification; CCI, Comprehensive Complication Index; n, number; SD, standard deviation.
In 35 patients, we detected major complications, defined as CDC ≥IIIb (22% of all complications) and minor complications, defined as CDC ≤IIIa, in 126 patients (78% of all complications). Among patients with major complications, we detected 19 anastomotic leakages (54% of all major complications) and 10 patients with severe pneumonia (29% of all major complications).
Confounder analysis showed two possible variables which had statistically significant impact on the rate of major complications: age >65 vs. ≤65 years and American Society of Anesthesiologists (ASA classification) III–IV vs. ASA I–II (Table 4).
Table 4
| Variables | N (%) | CR (%) | P (CR), Chi-squared test | CDC IIIb-V (%) | P (CDC), Chi-squared test | CCI, mean ± SD | P (CCI), U-Test |
|---|---|---|---|---|---|---|---|
| Age (years) | 0.001 | 0.150 | 0.001 | ||||
| ≤65 | 159 (57.0) | 49.7 | 10.1 | 13.7±18.6 | |||
| >65 | 120 (43.0) | 69.2 | 15.8 | 20.3±20 | |||
| ASA | 0.004 | 0.003 | 0.001 | ||||
| I–II | 175 (62.7) | 51.4 | 8 | 13.3±16.1 | |||
| III–IV | 104 (37.3) | 69.2 | 20.2 | 20.3±21.5 |
P<0.05 is considered to be significant. ASA, American Society of Anaesthesiologists; CR, complication rate; CDC, Clavien-Dindo-Classification; CCI, Comprehensive Complication Index; SD, standard deviation.
ASA I–II vs. ASA III–IV showed significant differences when applying CDC or CCI. Although there was no significant difference between the age groups regarding CDC, CCI showed significantly higher values for older patients.
No other confounder such as body mass index, sex, neoadjuvant therapy, histological subtype (adenocarcinoma vs. squamous cell carcinoma) number of resected lymph nodes, extended resection or surgical technique (open vs. hybrid) could be identified causing higher rates of complications besides age and ASA-classification.
To test whether age >65 years and ASA III–IV have an independent influence on LOS, we performed multivariant linear regressions analysis finding no significant influence on LOS. Therefore, direct comparison of CDC and CCI can be performed.
Correlation between LOS and CDC vs. CCI
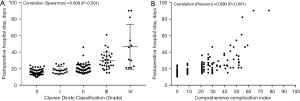
After esophagectomy CDC and CCI positively correlate with LOS, meaning more complications and more severe complications lead to longer LOS (Figure 1A,1B). CCI stronger correlates with LOS than CDC as the correlation coefficient from dependent samples was significantly higher [CCI (0.690) vs. CDC (0.609), P<0.001].
One vs. multiple complications after esophagectomy
Patients who experienced more than one complication have significantly prolonged LOS over patients who only experienced one complication (Figure 2A-2C). This effect was detectable even within patients who experienced several minor complications vs. ones who experienced only one minor complication (Figure 2A). However, the effect was more pronounced when only patients whose complications qualified as CDC III/IV were analyzed (Figure 2B) or when all patients with complications graded CDC II–IV were included (Figure 2C).

Discussion
For this study, we compared two complication scores regarding their predictive value on LOS after esophagectomy. Both indices were able to link complications to longer LOS. As we expected, CCI does correlate with LOS better than CDC, as more complications lead to longer hospitalization. As stated above, this has been shown before for major abdominal surgery, in gastric cancer surgery and surgery in inflammatory bowel disease (6-9), but also after hyperthermic intraperitoneal chemotherapy (12) or in related fields like urology after cystectomy (13).
Besides longer LOS in complicated courses, we found that older patients and patients with higher ASA-score have higher complication scores than younger and healthier ones, which is in line with Kim et al. who found a higher Charlson score as well as higher age to be risk factors for surgical complications after radical gastrectomy (8).
Classifying complications after surgery has many pitfalls. First, a normal postoperative course needs to be defined. Only thereafter deviations can be detected. This accounts especially for lower graded complications, as they deviate less clearly from the normal course and might also be documented less well (14). The importance of clearly defined regular postoperative courses as well as clear definitions of postoperative complications, especially the most common ones such as anastomic leakage, chyle leak, etc. were stated by Low et al. (15) in their 2015 consensus paper.
In severe complications handling may very well depend on the experience and qualification of the surgeon in charge as well as local standards. Complications can be treated in many ways, e.g., by endoscopic, radiological or surgical intervention and therefore the same complication may be rated as CDC IIIa, IIIb or even IVa with corresponding CCI. For example, anastomotic leakage can be handled endoscopically and therefore be classified as grade III complication or with reoperation, thus requiring general anesthesia and most likely ICU care, accounting for a grade IV complication.
Usually, LOS and higher grading of complications correlate positively, this may not always be the case as was described by Redden et al. who showed shorter LOS after thoracoscopic treatment of pleural empyema than after non-surgical treatment (16). Thus, LOS may occasionally not be the right parameter to judge management of complications in general. For example, Staiger et al. found a strong correlation of CCI and cost after surgery (17).
To address the problem of regularly occurring disabilities after major surgery, Dindo et al. excluded sequelae as well as failure to cure in their revision of the CDC (2). Sequelae are effects of surgery which account for morbidity, but are essential parts of the treatment, e.g., inability to eat large quantities after esophageal resection. For instance, routine endoscopic control of the anastomosis may be classified either as sequelae or even as a part of the surgery itself but should not account as a complication.
Finally, LOS does not only depend on medical parameters alone but also on social factors such as a prepared nursing service, availability of rehabilitation, medical resources at home or holidays which may not be documented.
After its development the CDC has been widely used to describe complications and has been proven to be simple, reproducible, logical, useful and comprehensive (2). As the CCI is based on the CDC the applicability of the CCI can be assumed to be just as good and reliable. In contrast, two urological groups found the CDC to have high interobserver variability and low accuracy especially in pediatric urology (18,19). The problem of interobserver discrepancies was addressed in this study by having all complications graded by a single experienced surgeon. Other scoring systems like the diagnose-based common terminology criteria for adverse events (CTCAE) system were found to be more complicated to apply than the CDC (12).
In conclusion, we could show that the correlation between CCI and LOS is significantly better than with CDC. Even in absence of major complications CCI was more precise in measuring the overall burden of complications in terms of LOS.
Besides the correlation of CCI and LOS, CCI provides a wider picture of the postoperative course of a patient and should therefore be used as the standard tool to measure postoperative complications. From our point of view CCI is primarily a scientific tool but is also valuable for monitoring postoperative courses of surgical interventions in single centers. A thorough monitoring of all complications, including all minor complications, should be implemented in routine clinical practice.
Acknowledgments
We thank Mr. Alexander Traut for providing us with the statistical analysis as well as graphs for our study.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://aoe.amegroups.com/article/view/10.21037/aoe-22-13/rc
Data Sharing Statement: Available at https://aoe.amegroups.com/article/view/10.21037/aoe-22-13/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoe.amegroups.com/article/view/10.21037/aoe-22-13/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Individual consent for this retrospective analysis was waived. No IRB approval statement or ethics vote was obtained as the study was purely retrospective, data was anonymously used for the study and no harm whatsoever may be caused by inclusion in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery 1992;111:518-26. [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Slankamenac K, Graf R, Barkun J, et al. The comprehensive complication index: a novel continuous scale to measure surgical morbidity. Ann Surg 2013;258:1-7. [Crossref] [PubMed]
- Téoule P, Bartel F, Birgin E, et al. The Clavien-Dindo Classification in Pancreatic Surgery: A Clinical and Economic Validation. J Invest Surg 2019;32:314-20. [Crossref] [PubMed]
- Katayama H, Kurokawa Y, Nakamura K, et al. Extended Clavien-Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today 2016;46:668-85. [Crossref] [PubMed]
- Veličković J, Feng C, Palibrk I, et al. The Assessment of Complications After Major Abdominal Surgery: A Comparison of Two Scales. J Surg Res 2020;247:397-405. [Crossref] [PubMed]
- de la Plaza Llamas R, Ramia Ángel JM, Bellón JM, et al. Clinical Validation of the Comprehensive Complication Index as a Measure of Postoperative Morbidity at a Surgical Department: A Prospective Study. Ann Surg 2018;268:838-44. [Crossref] [PubMed]
- Kim TH, Suh YS, Huh YJ, et al. The comprehensive complication index (CCI) is a more sensitive complication index than the conventional Clavien-Dindo classification in radical gastric cancer surgery. Gastric Cancer 2018;21:171-81. [Crossref] [PubMed]
- Zhu F, Feng D, Zhang T, et al. Toward a More Sensitive Endpoint for Assessing Postoperative Complications in Patients with Inflammatory Bowel Disease: a Comparison Between Comprehensive Complication Index (CCI) and Clavien-Dindo Classification (CDC). J Gastrointest Surg 2018;22:1593-602. [Crossref] [PubMed]
- Nimptsch U, Haist T, Krautz C, et al. Hospital Volume, In-Hospital Mortality, and Failure to Rescue in Esophageal Surgery. Dtsch Arztebl Int 2018;115:793-800. [Crossref] [PubMed]
- Ma G, Cao H, Wei R, et al. Comparison of the short-term clinical outcome between open and minimally invasive esophagectomy by comprehensive complication index. J Cancer Res Ther 2018;14:789-94. [Crossref] [PubMed]
- Dumitra S, O'Leary M, Raoof M, et al. The Comprehensive Complication Index: a New Measure of the Burden of Complications After Hyperthermic Intraperitoneal Chemotherapy. Ann Surg Oncol 2018;25:688-93. [Crossref] [PubMed]
- Haas M, Huber T, Pickl C, et al. The comprehensive complication index is associated with a significant increase in complication severity between 30 and 90 days after radical cystectomy for bladder cancer. Eur J Surg Oncol 2021;47:1163-71. [Crossref] [PubMed]
- Sethi MV, Zimmer J, Ure B, et al. Prospective assessment of complications on a daily basis is essential to determine morbidity and mortality in routine pediatric surgery. J Pediatr Surg 2016;51:630-3. [Crossref] [PubMed]
- Low DE, Alderson D, Cecconello I, et al. International Consensus on Standardization of Data Collection for Complications Associated With Esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg 2015;262:286-94. [Crossref] [PubMed]
- Redden MD, Chin TY, van Driel ML. Surgical versus non-surgical management for pleural empyema. Cochrane Database Syst Rev 2017;3:CD010651. [Crossref] [PubMed]
- Staiger RD, Cimino M, Javed A, et al. The Comprehensive Complication Index (CCI®) is a Novel Cost Assessment Tool for Surgical Procedures. Ann Surg 2018;268:784-91. [Crossref] [PubMed]
- Poletajew S, Zapała L, Piotrowicz S, et al. Interobserver variability of Clavien-Dindo scoring in urology. Int J Urol 2014;21:1274-8. [Crossref] [PubMed]
- Dwyer ME, Dwyer JT, Cannon GM Jr, et al. The Clavien-Dindo Classification of Surgical Complications is Not a Statistically Reliable System for Grading Morbidity in Pediatric Urology. J Urol 2016;195:460-4. [Crossref] [PubMed]
Cite this article as: Mathes A, Pauthner M, Haist T. Comparison of the Comprehensive Complication Index and Clavien-Dindo Classification for grading of postoperative complications after Ivor-Lewis esophagectomy in a high-volume center. Ann Esophagus 2023;6:40.


