
Multidisciplinary management of persistent dysphagia in mucous membrane pemphigoid: a case report
Introduction
Mucous membrane pemphigoid (MMP) is a group of chronic, autoimmune, subepithelial blistering disorders. Erosive lesions can appear on any combination of mucosal and cutaneous surfaces, and evolve into a characteristic scar, increasing patient morbidity. While eruptions are most common on oral and ocular mucosa, esophageal involvement is uncommon and can lead to debilitating stricture formation. Scantly available literature supports the combined use of immunosuppressive medications and esophageal dilations to achieve symptomatic control. Currently, no definitive management protocol exists for patients with esophageal lesions and uncontrolled symptoms particularly in the setting where dermatologic disease is well controlled (1,2). We are presenting a unique case of MMP with persistent dysphagia despite adequate immunosuppression successfully controlled with dermatology and gastroenterology co-management and with the use of topical swallowed steroid therapy. We present the following article in accordance with the CARE reporting checklist (available at https://aoe.amegroups.com/article/view/10.21037/aoe-20-24/rc).
Case presentation
We present the case of a 62-year-old male with known MMP and a reported 9-year history of relapsing painful lesions involving scalp, eyes, and mouth, as well as difficulty swallowing and eyelash loss. His medical history was significant for hypertension, diabetes, hypercholesterolemia, and gastroesophageal reflux disease (GERD). Medications included aspirin, metformin, metoprolol, simvastatin, omeprazole, sucralfate, and fluocinonide paste. He was evaluated by dermatologist after a trial of dapsone and 0.1% topical triamcinolone failed to alleviate symptomatic lesions.
On exam, there were several 5–15 cm wide pink, ovular, atrophic plaques on the left temporal scalp. The gums were edematous and erythematous but without erosions. There were many short and absent eyelashes, with scarring along the eyelid. Biopsy of the left scalp was submitted for histological review.
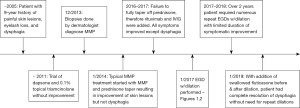
The diagnosis of MMP was confirmed, and the patient was placed on 60 mg prednisone daily and mycophenolate mofetil (MMF) 1,000 mg daily. Over the next 10 weeks, MMF was slowly increased to 4,000 mg daily and prednisone was tapered. The lesions on scalp, eyes and mouth improved; and the patient reported resolution of dysphagia during the next 7 months of treatment.
Unfortunately, once the dose of prednisone was decreased to 10 mg daily, oral lesions and dysphagia recurred. A single dose of rituximab infusion was given, prednisone was increased to 40 mg daily and the dose of MMF was maintained at 4,000 mg daily. Within 4 weeks, mucosal lesions demonstrated good healing. However, tapering the dose of prednisone once again led to recurrence of symptoms. Intravenous immunoglobulin (IVIG) therapy was then added to the regimen. Addition of IVIG resulted in complete resolution of all symptoms except dysphagia.
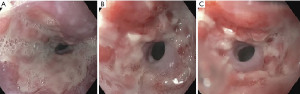
Endoscopy showed severe esophagitis and a stricture in the distal third of the esophagus (Figure 1). Over time, the stricture was dilated with good symptom control (Figure 2).
Over the next two years adequate control of mucocutaneous manifestations were achieved with the use of MMF 4,000 mg daily and occasional use of IVIG, rituximab and prednisone tapers but the symptoms of dysphagia persisted. Stricture dilation was performed numerous times during this period with the durability of symptomatic improvement lasting only 4–6 weeks.
Patient was subsequently referred to a GI specialist specializing in esophageal diseases for a second opinion. After careful review of his case, off-label, swallowed fluticasone 220 mcg twice daily was initiated before and after esophageal dilation. With the addition of topical esophageal therapy, the patient reported significant improvement in dysphagia and has been in clinical remission without need for repeat serial dilations and no additional GI follow-up needed (see timeline - Figure 3).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
MMP is a chronic, autoimmune, subepithelial blistering disease with a predilection for mucosal surfaces. It is characterized by the linear deposition of IgG, IgA, or C3 to a variety of antigens in the basement membrane. Patients often present with lesions in more than one site, including the mouth, eyelids, scalp, genitals, larynx, or esophagus (1). The evolution of active erosions into scars is the hallmark of this disease, which leads to loss of tissue function and increased patient morbidity. Esophageal involvement is seen in about 2–7% patients with MMP and can result in debilitating esophageal stricture and stenosis (2). Unfortunately, there is no definitive treatment for MMP and the goal of therapy is to reduce symptom burden and preserve function.
Since esophageal involvement is uncommon, accordingly there is a small collection of literature describing treatment for esophageal involvement in MMP, especially in the case of refractory disease. The First International Consensus on MMP categorized esophageal involvement as “high-risk” due to the life-threating sequelae of esophageal stricture and stenosis. For “high-risk” patients they favored initial treatment with prednisone (1.0–1.5 mg/kg per day) and cyclophosphamide (1–2 mg/kg per day) (1). More recent studies have explored prednisone with newer steroid-sparing immunomodulators alone or in series, including MMF (2 g/day), rituximab, anti-TNF-alpha agents, and IVIG to variable effect (2-7). In addition, the benefits of endoscopic dilation therapy have been well described in esophageal involvement, and can provide relief for patients whose dysphagia does not respond to systemic therapy (8-10).
The most recent case series from Zehou et al. describes the endoscopic findings and clinical course of 26 MMP patients with esophageal involvement and dysphagia. Patients with refractory symptoms were placed on cyclophosphamide or MMF for first-line treatment. Non-responders to this treatment received additional therapy with either rituximab or IVIG, during which other immunomodulators were held. In this study, only one patient failed to gain disease control despite treatment with rituximab, IVIG, and infliximab, and the authors do not describe future treatment strategies for this patient. The investigators did find that systemic immunomodulatory treatment significantly increased the time interval between dilation therapies (2).
To the best of our knowledge, our case is the first to describe the use of fluticasone swallow in a patient with refractory esophageal MMP despite treatment with maximal dose MMF combined with prednisone and alternating rituximab and IVIG. Though one may be limited by access to topical swallowed steroids their utility in this case is highlighted by the fact that the patient achieved excellent response, likely related to mucosal contact time of the swallowed steroids, without the additional risks and side effects of systemic steroids. Therefore, the addition of fluticasone swallow, in combination with balloon dilation therapy, successfully controlled our patient’s dysphagia and should be considered a treatment option for refractory disease. Though this condition is rare, future studies should be performed to evaluate the safety and efficacy profile of swallowed topical steroids in patients with MMP with consideration of their use for other autoimmune conditions affecting the esophagus.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://aoe.amegroups.com/article/view/10.21037/aoe-20-24/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoe.amegroups.com/article/view/10.21037/aoe-20-24/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Chan LS, Ahmed AR, Anhalt GJ, et al. The first international consensus on mucous membrane pemphigoid: definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol 2002;138:370-9. [Crossref] [PubMed]
- Zehou O, Raynaud JJ, Le Roux-Villet C, et al. Oesophageal involvement in 26 consecutive patients with mucous membrane pemphigoid. Br J Dermatol 2017;177:1074-85. [Crossref] [PubMed]
- Shetty S, Ahmed AR. Critical analysis of the use of rituximab in mucous membrane pemphigoid: a review of the literature. J Am Acad Dermatol 2013;68:499-506. [Crossref] [PubMed]
- Heelan K, Walsh S, Shear NH. Treatment of mucous membrane pemphigoid with rituximab. J Am Acad Dermatol 2013;69:310-1. [Crossref] [PubMed]
- Sánchez Prudencio S, Domingo Senra D, Martín Rodríguez D, et al. Esophageal Cicatricial Pemphigoid as an Isolated Involvement Treated with Mycophenolate Mofetil. Case Rep Gastrointest Med 2015;2015:620374. [Crossref] [PubMed]
- Neff AG, Turner M, Mutasim DF. Treatment strategies in mucous membrane pemphigoid. Ther Clin Risk Manag 2008;4:617-26. [Crossref] [PubMed]
- Kourosh AS, Yancey KB. Therapeutic approaches to patients with mucous membrane pemphigoid. Dermatol Clin 2011;29:637-41. [Crossref] [PubMed]
- Syn WK, Ahmed MM. Esophageal involvement in cicatricial pemphigoid: a rare cause of dysphagia. Dis Esophagus 2004;17:180-2. [Crossref] [PubMed]
- Furusawa K, Hasegawa T, Hirasawa Y, et al. Mucous membrane pemphigoid with esophageal stricture treated with balloon dilatation. J Dermatol 2015;42:325-7. [Crossref] [PubMed]
- Warren LJ, Wojnarowska F, Wilkinson JD. Oesophageal involvement in cicatricial pemphigoid. Australas J Dermatol 1997;38:148-51. [Crossref] [PubMed]
Cite this article as: Garcia P, Mattessich S, Sao R, Lu J, Rezaizadeh H. Multidisciplinary management of persistent dysphagia in mucous membrane pemphigoid: a case report. Ann Esophagus 2023;6:34.



