
A narrative review of the function of upper esophageal sphincter in the achalasia
Introduction
Achalasia is the most common primary motility disorder of the esophagus with an incidence of 1 per 100,000 (1). The main symptoms are weight loss, dysphagia, regurgitation, and chest pain. Achalasia is defined by the presence of elevated integrated relaxion pressure and is divided into subtypes according to the different patterns of non-peristaltic esophageal pressure (2). Conventional manometry has been used to evaluated disorders mainly of the esophageal body and lower esophageal sphincter (LES), but with the advent of high-resolution manometry (HRM) the upper esophageal sphincter (UES) became of interest in the last years (3) and now has its value in the pathophysiology of achalasia as well.
The objective of the article is to review of the alterations of UES in the achalasia under the optics of HRM. We present the following article in accordance with the Narrative Review reporting checklist (available at https://aoe.amegroups.com/article/view/10.21037/aoe-21-14/rc).
Methods
The research has been done from PubMed with the following key words: upper esophageal sphincter, achalasia, and high-resolution manometry. Only articles written in English performed on adult humans were selected for primary review. The references of the articles were manually reviewed for additional relevant papers.
Discuss
UES tonus in achalasia
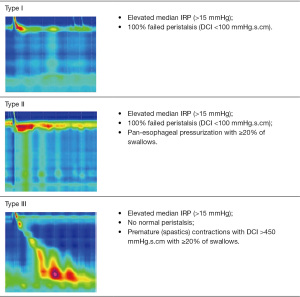
Basal pressure of the UES can vary (ranging from hypotensive, normotensive, to hypertensive) according to the esophageal pressurization (4-8), that represents in fact subtypes of achalasia according to the Chicago Classification (2) (Figure 1). Subtypes with esophageal pressurization (achalasia type II and III) usually present with elevated basal pressure of the UES when compared to the non-pressurized subtype (achalasia type I) (4,6,8).
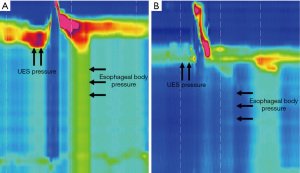
The residual pressure of UES is elevated in achalasia patients, but in patients with esophageal pressurization this value is even bigger (Figure 2) (4,6,8).
This increase of the basal and residual pressures of UES in achalasia are related the reflex mechanism of esophagus to decrease the aspiration of undigested food and saliva (4,6).
The swallowing and UES in patients with achalasia
Patients with achalasia have decreased esophageal clearance due to progressive myenteric neuron loss, what promote decreased of LES relaxation and aperistalsis (9,10). In addition, there is an increase of residual pressure of the UES and higher thoracic pressure, which increase the esophageal pressure (8). In order to overcome this hostile environment, the patient with achalasia involuntarily performs an effortful swallowing characterized by short pharyngeal contractions that are also hypertonic and premature in relation to UES relaxation, aiming to facilitate the transport of the bolus into the stomach (4).
The importance of UES in esophageal pressurization
UES pressure directly influences esophageal pressure. Two theories can explain the relationship between esophageal body and UES. First, the simultaneous contraction or pressurization of esophageal body induce a viscous resistance of bolus and reflex response in UES, increasing its basal and residual pressure (9). The esophageal pressure is determinate by the degree of esophageal body pressurization, and type I achalasia would be an advanced stage of type II and III disease, because of progressive myenteric neuron loss (10). Therefore, in patients with type I achalasia, the esophageal body pressure is low, and induces low myenteric reflex response resulting in low residual and basal pressure of the UES, in patients with type II and III achalasia, the esophageal body pressure is high, and induces a high myenteric reflex response resulting in high residual and basal pressure of the UES (9).
As second theory, esophageal pressurization is not caused by muscular contraction because: (I) pressure are the identical along the whole extension of the wave, the muscles can not to contract with such precision; moreover, the contraction transition zone is absent; (II) the esophagus is denervated, even so may induce tertiary spontaneous contractions; waves coordinated with deglutition are not feasible; but, idiopathic achalasia may conserve excitatory nerves allowing spastics contractions (type III achalasia); (III) shortening of the esophagus does not appear in HRM (8). In this case, the UES plays an important role in the genesis of pressurized waves, with interaction thoracic pressure allowing the pressurization and promoting esophageal emptying. The UES basal and residual pressure is hypertonic to sustain the higher thoracic pressure, and an effortful swallow with decreased relaxation increase even more the esophageal pressure, in a fluid-filled esophagus. These unconscious reflexes may help to force the food into the stomach overcoming a non-functional barrier at the esophagogastric junction (8). This mechanism is changed after treatment of achalasia (5,11-13).
The UES after treatment of achalasia
Achalasia treatment [esophageal dilatation, peroral endoscopic myotomy (POEM) or myotomy] increase esophageal emptying. Some studies have shown that UES parameters may return to normality after treatment (5,11-13).
The outcomes of achalasia treatment are related to Chicago Classification. Type II achalasia has a better prognosis compared the type I and III (14). Some studies suggest that abnormalities of UES (hypertonia and high residual pressure) in patients with achalasia determine a poor prognosis of the treatment. These authors think that the poorer response is associated abnormalities of the UES, that are due to a compensatory and protective effect in consequence of inadequate esophageal emptying and regurgitation, that occur mainly in cases of advances diseases (12,13).
Conclusions
The UES is altered in achalasia, with increase of its residual and basal pressure, that is related to the degree of esophageal pressurization. These abnormalities can be result or even the cause of esophageal body pressurization and can be directly related to a poor result of achalasia treatment.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Esophagus for the series “Upper Esophageal Sphincter”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://aoe.amegroups.com/article/view/10.21037/aoe-21-14/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoe.amegroups.com/article/view/10.21037/aoe-21-14/coif). The series “Upper Esophageal Sphincter” was commissioned by the editorial office without any funding or sponsorship. FAMH served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Esophagus from September 2020 to August 2022. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Podas T, Eaden J, Mayberry M, et al. Achalasia: a critical review of epidemiological studies. Am J Gastroenterol 1998;93:2345-47. [Crossref] [PubMed]
- Kahrilas PJ, Bredenoord AJ, Fox M, et al. The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 2015;27:160-74. [Crossref] [PubMed]
- Ayazi S, Crookes PF. High-resolution esophageal manometry: using technical advances for clinical advantages. J Gastrointest Surg 2010;14:S24-32. [Crossref] [PubMed]
- Menezes MA, Herbella FA, Patti MG. High-Resolution Manometry Evaluation of the Pharynx and Upper Esophageal Sphincter Motility in Patients with Achalasia. J Gastrointest Surg 2015;19:1753-7. [Crossref] [PubMed]
- Ren Y, Tang X, Chen F, et al. Myotomy of Distal Esophagus Influences Proximal Esophageal Contraction and Upper Esophageal Sphincter Relaxation in Patients with Achalasia After Peroral Endoscopic Myotomy. J Neurogastroenterol Motil 2016;22:78-85. [Crossref] [PubMed]
- Blais P, Patel A, Sayuk GS, et al. Upper esophageal sphincter (UES) metrics on high-resolution manometry (HRM) differentiate achalasia subtypes. Neurogastroenterol Motil 2017;29: [Crossref] [PubMed]
- Triantafyllou T, Theodoropoulos C, Mantides A, et al. Can the upper esophageal sphincter contractile integral help classify achalasia? Ann Gastroenterol 2018;31:456-61. [Crossref] [PubMed]
- Anefalos A, Herbella FAM, Patti MG. Upper Esophageal Sphincter Motility and Thoracic Pressure are Determinants of Pressurized Waves in Achalasia Subtypes According to the Chicago Classification. World J Surg 2020;44:1932-8. [Crossref] [PubMed]
- Ren Y, Ke M, Fang X, et al. Response of esophagus to high and low temperatures in patients with achalasia. J Neurogastroenterol Motil 2012;18:391-8. [Crossref] [PubMed]
- Kahrilas PJ, Boeckxstaens G. The spectrum of achalasia: lessons from studies of pathophysiology and high-resolution manometry. Gastroenterology 2013;145:954-65. [Crossref] [PubMed]
- Wauters L, Van Oudenhove L, Selleslagh M, et al. Balloon dilation of the esophago-gastric junction affects lower and upper esophageal sphincter function in achalasia. Neurogastroenterol Motil 2014;26:69-76. [Crossref] [PubMed]
- Mathews SC, Ciarleglio M, Chavez YH, et al. Upper esophageal sphincter abnormalities are strongly predictive of treatment response in patients with achalasia. World J Clin Cases 2014;2:448-54. [Crossref] [PubMed]
- Chavez YH, Ciarleglio MM, Clarke JO, et al. Upper esophageal sphincter abnormalities: frequent finding on high-resolution esophageal manometry and associated with poorer treatment response in achalasia. J Clin Gastroenterol 2015;49:17-23. [Crossref] [PubMed]
- Pandolfino JE, Kwiatek MA, Nealis T, et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 2008;135:1526-33. [Crossref] [PubMed]
Cite this article as: Menezes MDA, Valezi AC, Herbella FAM. A narrative review of the function of upper esophageal sphincter in the achalasia. Ann Esophagus 2022;5:28.


