Colon interposition in the management of post-corrosive strictures
Introduction
The ingestion of chemical agents is a rare but potentially fatal event and nowadays it represents a worldwide public health problem, usually seen in the younger age group (1). Ammonium hydroxide found in cleaning products, sodium hypochlorite used in bleach and potassium, sodium hydroxide found in cleaners and hair products, and hydrochloric acid used for toilet bowl are the caustic substances most frequently ingested at home (2).
The 2018 annual report presented by the American Association of Poison Control Centres (AAPCC) (3) describes 84,000 cases of exposure to corrosive/toxic agents with an annual increase of 4.45% in major adverse events. In 80% of cases, people involved are children aged 2–6 who accidentally ingest products used for domestic cleaning, but they usually report minor injuries. In the remaining 20% of cases, adults aged between 30–40 years voluntarily take some corrosive substances for suicidal purpose. These patients are at risk of potentially fatal injuries (3), because they usually intake a greater amount of substance.
The pH of caustic agents impact on the severity of sequelae. Strong acids with pH values below 2 and bases with pH above 10 are responsible for the most severe lesions. Severity of the clinical picture also depends on volume ingested, time of exposition, physical state, concentration and volume of the toxic agent. Usually, acids cause a mucosal damage because denature proteins with coagulation necrosis; the coagulum prevents the acid from reaching deeper tissues limiting the damage at the mucosal layer, but injuries can be severe. Basic substances can cause full-thickness wounds, because they saponify fats and create liquefaction necrosis, allowing deep penetration and extending tissue damage.
In clinical practice, in the acute phase (first 1–3 days) the most severe and frequent complication is visceral necrosis and/or perforation. Instead, after one/two weeks the repair process promotes the connective tissue production and, later, the scar retraction (4,5).
Clinical effects of caustic ingestions are immediate; only survivors of an acute episode are liable to suffer for delayed manifestations.
Late sequelae of the gut that can occur after variable time, are disabling and can be life-threatening (fistulas, strictures, malignancy). Because of the large diameter of the stomach, gastric strictures are uncommon; many patients have concomitant gastro-oesophageal strictures (6). Contrariwise, strictures can often involve the oesophagus; they can be long, complex and complicated, occur over a period of weeks to months, have a long stabilisation delay (7) and lead to chronic pain and malnutrition (1). Both emergency endoscopy (8,9) and CT (10) reliably predict their development; antibiotics (11) and steroids (12,13) failed to prevent delayed strictures. Repeated endoscopic dilatation still remains the first-line management and can be effective in half of patients (11). However, after five to seven sessions of dilatations, surgical replacement of the esophagus must be considered (14), although you need to consider it carefully because acute and chronic severe complications may burden surgery outcomes. Strictures can often involve both esophagus and stomach, so a colonic graft is the method of reconstruction used in most patients.
In this article, we present the main step of preoperative, intraoperative and postoperative pathway according to our twenty-year experience on colonic graft in esophageal reconstruction for caustic strictures.
The choice of the esophageal substitute
When patients have a healthy stomach, you have to take into account that an esophago-gastroplasty has many theoretical advantages: it requires a single anastomosis only, has less perioperative complications and offers best functional results. Unfortunately, it requires a partial or a total removal of the scarred esophagus and this is not always possible without a high risk of major complications (bleeding, tracheal injuries) (15-17). For these reasons, only selected patients can be submitted to an esophago-gastroplasty.
Colon interposition for esophageal replacement is more frequently performed for treatment of caustic burns (18-22). The first question is: which is the best colonic segment to use? To date, the question is still debated, because reported series are not homogeneous. Before to perform the choice between right colon and left colon, some anatomical, functional and single patient aspects must be considered. The first key point is to perform a colonic interposition with a good vascular support. In this purpose, the colonic peduncle and the marginal artery play an important role, because ischemia is the main cause of failure of the surgical treatment. Some authors (23-26) describe a not negligible anatomical variability in the vascular anatomy of the right colon. In their autoptic and arteriographic studies, Peters (27) and Stewart (28) reported that a normal right marginal artery was founded in 30–95% of cases, while conversely the presence of a regular left marginal artery was generally guaranteed. So, based on these findings, some authors claimed that the left colon is the first choice for replacing a scared esophagus and using the right colon is hazardous (29,30). In contrast, others (31) viewed some advantages using the right colon, especially when the ileo-caecal valve was preserved, because the valve seems to prevent the reflux. In addition, in case of vascular failure of the right graft, it is always possible to use the left colon, but not the opposite. Unfortunately, randomized controlled studies never investigated if right or left colon is the best substitute of the scared esophagus, and papers from high-volume centers showed overlapping results (6).
In order to establish the vascular support of right and left colon, and minimize the risk of colonic necrosis, some authors advocated preoperative arteriography (19,25,27). We also, in our experience of 12 patients, performed preoperative arteriography in all cases. The vascular preoperative examination surely allows an accurate picture of anatomical vascularization; however, it is not able to define the effective blood supply of the graft, which is verifiable only after intraoperative, reversible clamp of the vascular pedicle. In our opinion, this test must be performed twice, before and after the trans-thoracic (or retrosternal) pull-up of the colonic graft.
Route of reconstruction and surgical timing
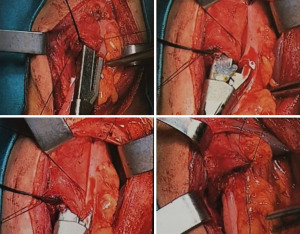
The substernal tunnel is the route of choice because the use of posterior mediastinum needs the ablation of the scared esophagus that may be often difficult and hemorrhagic (Figure 1). In order to avoid compression of the transposed colon, especially when the thoracic inlet is narrow, a partial sternotomy is indicated. In our experience, we systematically perform resection of the sternal manubrium. Using the substernal route, some investigators reported an increased risk of cervical anastomotic leak (19,32). Time for operation after corrosive injury is still under controversy. In his study on rats, Bassiouny (33) demonstrated that scaring continued for 6 months after corrosive event of esophagus. So, surgical intervention must be performed after almost 6 months from the acute event, in order to prevent the risk of anastomotic stenosis promoted by a too earlier operation, when the scar is not completely formed.

Early complications
Mortality of colon interposition ranges between 0% and 10% and about 19–63% of patients undergoing colic transposition surgery reported some postoperative complications (6). The incidence of intraoperative death has decreased over time, because of improved preoperative preparation, surgical technique, postoperative care and patient selection. Colonic necrosis represents the most dangerous complication (0–14%) and the major cause of death following this procedure; the other most dangerous complication is the cervical anastomotic leak (6–28%) (6).
Vascular impairment is usually complicated by venous insufficiency and thrombosis, and less frequently, by arterial insufficiency. This problem is then amplified by bacterial contamination of the colon, and results in necrosis of the transposed colic segment in more than 14% of patients, with a significantly higher incidence than that seen for esophageal-to-stomach replacement (1%) (34). If not immediately recognized and treated with removal of the colic graft, this complication is fatal.
Usually, anastomosis dehiscence occurs at the cervical level. In contrast, dehiscence at the level of the colonic-gastric, ileo-gastric, colonic-colonic anastomosis is uncommon. As for all anastomoses of the gastrointestinal tract, the origin of failure in colic transposition is multifactorial, including ischemia, technical errors, anastomosis tension, infection. Therapy consists of resting the anastomosis by using parenteral nutrition, adequate drainage, and administration of antibiotic therapy. In the absence of total detachment of the anastomosis, proximal colic necrosis, or mediastinitis, surgical intervention is rarely required.
Late complications
Late complications after esophageal reconstruction are common, occurring in half of patients (14). Usually as a late complication of an anastomotic leakage, stenosis of the cervical anastomosis is the most common event (4–59%). Many fistulas spontaneously heal, but more than 50% are complicated by the onset of anastomotic stenosis requiring subsequent dilatation. Repeated surgery for revision of the anastomosis is rare.
Other complications are not so frequent, but redundancy, ulceration, reflux, and cancer of the graft can burden functional results and quality of life (35-39). In 2000, Orringer (40) described a side-to-side stapled anastomosis that allows the creation of wide cervical anastomoses that are unlikely to develop stenosis (Figure 2).
Peptic ulceration occurs in 0.5% to 8% of patients. The common factor in the eleven cases reviewed by Malcolm (41) was the location of the colonic-gastric anastomosis at the level of the anterior wall of the stomach. Belsey (42) emphasized the importance of packing the colonic-gastric anastomosis at the level of the posterior gastric wall (a technique commonly adopted by our group) to avoid complications of a peptic nature. Despite this technique, in Belsey’s experience 10% of patients undergoing colic transposition, developed stenosis of the colonic-gastric anastomosis which required surgical revision. In our experience, gastrocolic reflux caused relevant alterations of the colonic graft in one patient only (Figure 3).
Redundancy of the transposed colonic segment is uncommon in short-segment colic transpositions but is an unavoidable problem when long segment of colon is transposed. Specific maneuvers can reduce the innate tendency of the colon to dilate and become tortuous. Failure to reduce the excesses of the cervical and thoracic portions of the colic graft within the chest and abdomen is a common cause of this primary complication. The predisposition of the thin wall of the colon to dilate because of negative pressure within the thorax and the absence of peristalsis may promote dilatation despite the use of a colic segment of adequate length. The distance of the transposed colic segment from the vascular pedicle, due to intrinsic redundancy, results in significant failure after a long time.
Jeyasingham et al. (43) reported an estimated 25% significant colonic redundancy in 69 patients followed for a period of 30 years after long-segment colic transposition. In such circumstances, reoperation may be required to correct the complications of colic transposition. Treatment of persistent symptoms and anastomotic complications by reintervention are reported in more than 37% of cases. In our series, only one patient developed a redundancy of colonic-gastric anastomosis 11 years after the transposition surgery and needed a reoperation.
Development of adenocarcinoma at the level of the transposed colic segment is infrequent, with <10 cases reported in literature (44). It may be related to the effect of gastric acid content or bile on colonic mucosa, occurring 5–47 years after surgery (44). Dysfunctional disorders of the transposed colic segment result in persistent dysphagia or in the development of upper gastrointestinal and respiratory tract symptoms. Good to excellent results have been obtained with colic transposition in 75–85% of patients with benign esophageal pathology. In a review of 45 patients treated for benign disease with colic transposition, 24% had no gastrointestinal symptoms at follow-up. Regurgitation, vomiting, and dumping syndrome occurred in 22%, 31%, and 18% of patients, respectively (45).
Mucocele of the excluded esophagus is also a rare reported complication. In our experience, we successfully treated one patient in a conservative way [three-stage ethanol ablation (46)].
Functional results
The best indicator of successful colic transposition is a patient’s ability to gain and maintain weight. In children, this ability can be monitored as they grow. Stone et al. (47) reported that 89% of 36 children who underwent colic transposition increased their percentile weight. Colic transposition resulted in an increase in percentile weight in children with esophageal atresia, ranging from the 12th to 33rd percentile on average, and maintenance of the 50th percentile in children with alkali stenosis. In 5 or 6 children undergoing colic transposition, a reduction in fat absorption was called into account for limited weight gain. Quality of life improved in patients treated for esophageal atresia with both primary repair and colic transposition. Patients undergoing primary repair showed quality-of-life indices similar to control cases, whereas those undergoing colic transposition showed a lower quality of life because of the development of digestive and respiratory symptoms.
Coevoet (48) compared quality of life of 80 patients submitted to colonic interposition with a reference group of patients undergone gastric tube, using the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30, EORTC QLQ-OG25 and Swallowing Quality of Life (SWAL-QOL) questionnaire scores. About 65% of patients reported good long-term results despite the high complication rate and the severity of the disease.
Functional study
Functional assessment of the interposed colic segment using fluoroscopy, cineradiography, and manometric studies leads to the conclusion that transit through the colon is predominantly passive and gravity-dependent and that the transposed organ does not appear to develop any motor activity.
Knowledge of the peristaltic activity at the level of the interposed colic segment is important since the decision to place the colic graft in an iso-peristaltic or anti-peristaltic direction depends on the presence or absence of a propulsive colonic motor activity. Belsey (42) stated that the long-term clinical results of anti-peristaltic colic transposition are not satisfactory. The reported manometric results support the notion that a good intraluminal colonic motor response to water is present, but conflicting results are not observed in patients submitted to an anti-peristaltic transposition.
For more than 20 years, there has been a growing interest regarding the use of radionuclide techniques for the study of esophageal motility. The common point of view is that the presence of a normal proximal segment of the esophagus acts as a propulsive thrust, facilitating transit through the transposed colic segment. However, we can assume that the colon as a substitute for the esophagus, with reliable peristaltic contractions, takes part actively in the transit of the bolus. Drawing inspiration from the observations made, in terms of altered permeability, on patients with chronic inflammatory bowel disease, we wanted to subject these patients to 51Cr-EDTA test. We noticed the appearance of altered intestinal permeability in the follow-up.
These results, although not compared with further metabolic and morphological findings, lead us to hypothesize a possible long-term reabsorption of substances potentially capable of damaging liver and kidneys. In this regard, we suggest to evaluate, in the long follow-up, any metabolic and/or morphological alterations apparently not correlated with the interposition of a colic loop in the upper digestive district.
Conclusions
Esophageal-colon-gastroplasty is proved to be effective in the treatment of stenotic complications following caustic intake. Waiting for randomized controlled studies, surgeon’s experience is the most important factor to choose right or left colon as esophageal substitute. Considering the high rate of severe complications, surgery must be performed in high-volume hospitals.
Age, psychiatric disorders, massive ingestion, emergency tracheotomy, extended visceral resections, short delays in reconstruction, and pharyngeal involvement worsen surgical outcomes.
In our opinion, follow-up of these patients should not tend only to verify the patency of the transit and weight maintenance, but it should identify any lesion of the graft and any metabolic alteration referring to an altered permeability of the transposed colic segment.
Because it is not always possible to trace the exact dynamic of caustic intake and to reveal the suicidal purposes, a long-term psychologic support must be always considered.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Annals of Esophagus for the series “Management of Esophageal Perforations and Injuries and Other Benign Diseases”. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://aoe.amegroups.com/article/view/10.21037/aoe-2020-27/coif). The series “Management of Esophageal Perforations and Injuries and Other Benign Diseases” was commissioned by the editorial office without any funding or sponsorship. VP served as an unpaid Guest Editor of the series. DN served as an unpaid Guest Editor of the series and serves as an unpaid editorial board member of Annals of Esophagus from October 2019 to September 2021. All authors have no other conflicts of interest to declare.
Ethical Statement: All authors are accountable for all aspects of this work in ensuring that questions related to the accuracy or integrity of any part of this work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Johnson CM, Brigger MT. The public health impact of pediatric caustic ingestion injuries. Arch Otolaryngol Head Neck Surg 2012;138:1111-5. [Crossref] [PubMed]
- Hoffman RS, Burns MM, Gosselin S. Ingestion of Caustic Substances. N Engl J Med 2020;382:1739-48. [Crossref] [PubMed]
- Gummin DD, Mowry JB, Spyker DA, et al. 2018 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 36th Annual Report. Clin Toxicol (Phila) 2019;57:1220-413. [Crossref] [PubMed]
- Bautista A, Varela R, Villanueva A, et al. Motor function of the esophagus after caustic Burns. Eur J Pediatr Surg 1996;6:204-7. [Crossref] [PubMed]
- Chen YJ, Chen CC, Chen TH, et al. The association between caustic ingestion and psychiatric comorbidity based on 396 adults within 20 years. Risk Manag Healthc Policy 2020;13:1815-24. [Crossref] [PubMed]
- Chirica M, Bonavina L, Kelly MD, et al. Caustic ingestion. Lancet 2017;389:2041-52. [Crossref] [PubMed]
- Lahoti D, Broor SL, Basu PP, et al. Corrosive esophageal strictures: predictors of response to endoscopic dilation. Gastrointest Endosc 1995;41:196-200. [Crossref] [PubMed]
- Cheng HT, Cheng CL, Lin CH, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol 2008;8:31. [Crossref] [PubMed]
- Zargar SA, Kochhar R, Mehta S, et al. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest Endosc 1991;37:165-9. [Crossref] [PubMed]
- Ryu HH, Jeung KW, Lee BK, et al. Caustic injury: can CT grading system enable prediction of esophageal stricture? Clin Toxicol (Phila) 2010;48:137-42. [Crossref] [PubMed]
- Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol 2013;19:3918-30. [Crossref] [PubMed]
- Fulton JA, Hoffman RS. Steroids in second degree caustic burns of the esophagus: a systematic pooled analysis of fifty years of human data: 1956-2006. Clin Toxicol (Phila) 2007;45:402-8. [Crossref] [PubMed]
- Anderson KD, Rouse TM, Randolph JG. A controlled trial of corticosteroids in children with corrosive injury of the esophagus. N Engl J Med 1990;323:637-40. [Crossref] [PubMed]
- Chirica M, Veyrie N, Munoz-Bongrand N, et al. Late morbidity after colon interposition for corrosive esophageal injury: risk factors, management, and outcome. A 20-years experience. Ann Surg 2010;252:271-80. [Crossref] [PubMed]
- Wu MH, Lai WW. Esophageal reconstruction for esophageal strictures or resection after corrosive injury. Ann Thorac Surg 1992;53:798-802.
- Gupta NM, Gupta R. Transhiatal esophageal resection for corrosive injury. Ann Surg 2004;239:359-63. [Crossref] [PubMed]
- Young MM, Deschamps C, Allen MS, et al. Esophageal reconstruction for benign disease: self-assessment of functional outcome and quality of life. Ann Thorac Surg 2000;70:1799-802. [Crossref] [PubMed]
- Gossot D, Azoulay D, Piriou P, et al. Mortality and morbidity after use of the colon as esophageal substitute. A study of 105 patients. Gastroenterol Clin Biol 1990;14:977-81.
- DeMeester TR, Johansson KE, Franze I, et al. Indications, surgical technique, and long-term functional results of colon interposition or by-pass. Ann Surg 1988;208:460-74. [Crossref] [PubMed]
- Mansour KA, Curtis Bryan F, Carlson GW. Bowel interposition for esophageal replacement: twenty-five years’ experience. Ann Thorac Surg 1997;64:752-6. [Crossref] [PubMed]
- Yararbai O, Osmanodlu H, Kaplan H, et al. Esophagocoloplasty in the management of postcorrosive strictures of the esophagus. Hepatogastroenterology 1998;45:59-64.
- Fürs H, Hartl WH, Lohe F, et al. Colon interposition for esophageal replacement. An alternative technique based on the use of the right colon. Ann Surg 2000;231:173-8. [Crossref] [PubMed]
- Sonneland J, Anson BJ, Beaton LE. Surgical anatomy of the arterial supply to the colon from the superior mesenteric artery based upon a study of 600 specimens. Surg Gynecol Obstet 1958;106:385-98.
- Yamaguchi S, Kuroyanagi H, Milsom JW, et al. Venous anatomy of the right colon: precise structure of the major veins and gastrocolic trunk in 58 cadavers. Dis Colon Rectum 2002;45:1337-40. [Crossref] [PubMed]
- Ventemiglia R, Khalil KG, Frazier OH, et al. The role of preoperative mesenteric arteriography in colon interposition. J Thorac Cardiovasc Surg 1977;74:98-104.
- Ribet M, Barrat C. Colonic esophagoplasty for benign lesions. Ann Chir 1995;49:133-7.
- Peters JH, Kronson JW, Katz M, et al. Arterial anatomic considerations in colon interposition for esophageal replacement. Arch Surg 1995;130:858-62; discussion 862-3. [Crossref] [PubMed]
- Stewart JARF. Blood supply of the large intestine. Arch Surg 1933;26:843-91.
- Gerzic ZB, Knezevic JB, Milicevic MN, et al. Esophagocoloplasty in the management of postcorrosive strictures of the esophagus. Ann Surg 1990;211:329-36.
- Thomas P, Fuentes P, Giudicelli R, et al. Colon interposition for esophageal replacement: current indications and long-term function. Ann Thorac Surg 1997;64:757-64.
- Bothereau H, Munoz-Bongrand N, Lambert B, et al. Esophageal reconstruction after caustic injury: is there still a place for right coloplasty? Am J Surg 2007;193:660-4. [Crossref] [PubMed]
- Mitchell IM, Goh DW, Roberts KD, et al. Colon interposition in children. Br J Surg 1989;76:681-6. [Crossref] [PubMed]
- Bassiouny IE, Al-Ramadan SA, Al-Nady A. Long-term functional results of transhiatal oesophagectomy and colonic inter- position for caustic oesophageal stricture. Eur J Pediatr Surg 2002;12:243-7. [Crossref] [PubMed]
- Javed A, Pal S, Dash NR, et al. Outcome following surgical management of corrosive strictures of the esophagus. Ann Surg 2011;254:62-6. [Crossref] [PubMed]
- Hsieh YS, Huang KM, Chen TJ, et al. Metachronous adenocarcinoma occurring at an esophageal colon graft. J Formos Med Assoc 2005;104:436-40.
- Cheng YJ, Li HP, Kao EL. Perforated diverticulum: rare complication of interposed substernal colon. Ann Thorac Surg 2006;82:717-9. [Crossref] [PubMed]
- de Delva PE, Morse CR, Austen WG Jr, et al. Surgical management of failed colon interposition. Eur J Cardiothorac Surg 2008;34:432-7. [Crossref] [PubMed]
- Domreis JS, Jobe BA, Aye RW, et al. Management of long-term failure after colon interposition for benign disease. Am J Surg 2002;183:544-6. [Crossref] [PubMed]
- Strauss DC, Forshaw MJ, Tandon RC, et al. Surgical management of colonic redundancy following esophageal replacement. Dis Esophagus 2008;21:E1-5. [Crossref] [PubMed]
- Orringer MB, Marshall B, Iannettoni MD. Eliminating the cervical esophagogastric anastomotic leak with a side-to-side stapled anastomosis. J Thorac Cardiovasc Surg 2000;119:277-88.
- Malcolm JA. Occurrence of peptic ulcer in colon used for esophageal replacement. J Thorac Cardiovasc Surg 1968;55:763-72.
- Belsey R. Reconstruction of the esophagus with left colon. J Thorac Cardiovasc Surg 1965;49:33-55.
- Jeyasingham K, Lerut T, Belsey RH. Functional and mechanical sequelae of colon interposition for benign oesophageal disease. Eur J Cardiothorac Surg 1999;15:327-31; discussion 331-2. [Crossref] [PubMed]
- Barbosa B, Santos B, Mesquita I, et al. Adenocarcinoma arising in a colonic interposition after esophagectomy for benign stricture and review of the literature. J Surg Case Rep 2018;2018:rjy264. [Crossref] [PubMed]
- Isolauri J, Harju E, Markkula H. Gastrointestinal symptoms after colon interposition. Am J Gastroenterol 1986;81:1055-8.
- Nachira D, Chiappetta M, Congedo MT, et al. Successful Three-Stage Ethanol Ablation of Esophageal Mucocele. J Vasc Interv Radiol 2016;27:152-4. [Crossref] [PubMed]
- Stone MM, Fonkalsrud EW, Mahour GH, et al. Esophageal replacement with colon interposition in children. Ann Surg 1986;203:346-51. [Crossref] [PubMed]
- Coevoet D, Van Daele E, Willaert W, et al. Quality of life of patients with a colonic interposition post-oesophagectomy. Eur J Cardiothorac Surg 2019;55:1113-20. [Crossref] [PubMed]
Cite this article as: Porziella V, Tabacco D, Zanfrini E, Evangelista J, Vita ML, Petracca-Ciavarella L, Pogliani L, Meacci E, Congedo MT, Chiappetta M, Margaritora S, Nachira D. Colon interposition in the management of post-corrosive strictures. Ann Esophagus 2023;6:12.