
Minimally invasive McKeown esophagectomy: a narrative review of current operative and oncologic outcomes
Introduction
The first report of resection of the thoracic esophagus was published in 1913 by Torek (1). The patient remained in permanent discontinuity with a cervical esophagostomy and abdominal gastrostomy. It was not until 1933 that the first successful transhiatal esophagectomy was performed, using a cervicoabdominal gastric pull-up method (2), followed in 1938 by esophagectomy and esophagogastrostomy (3). During this time, advances in anesthesia allowed for transthoracic resection of the esophagus. In 1946, Lewis reported a two-field operation that involved laparotomy and mobilization of the stomach, right thoracotomy and resection of the esophagus, and completion of a thoracic esophagogastric anastomosis (4). This transthoracic approach with intrathoracic esophagogastric anastomosis then became the standard technique of esophageal resection and reconstruction.
Three-field esophagectomy was first reported by McKeown in the 1970s and involves dissection in both the chest and the abdomen, along with a cervical neck anastomosis (5). Traditionally, thoracotomy was used for esophageal mobilization, laparotomy for gastric mobilization, and then left neck incision to fashion the cervical anastomosis. To this day, indications for three-field esophagectomy include midesophageal tumors, long-segment Barrett’s disease, and benign diseases such as dysmotility disorders. Common complications of this operation include atrial arrythmias and pneumonia; severe morbidity can result from recurrent laryngeal nerve injury and anastomotic leak or stricture (6).
The major advantage of McKeown esophagectomy is the more straightforward management of cervical anastomotic leak, with decreased morbidity—intrathoracic anastomotic leak, which can follow transhiatal esophagectomy, is generally more difficult to manage. However, three-hole esophagectomy is not without its own associated morbidity, which includes respiratory insufficiency after combined thoracic and abdominal incisions. For this reason, to avoid thoracotomy, Orringer repopularized transhiatal esophagectomy (7). At present, McKeown esophagectomy is still widely used in clinical practice, and application has gained traction in line with the advances in minimally invasive technique, anesthesia, and postoperative care (8). This review will report on the minimally invasive approaches used at our institution and elsewhere, describe the historical evolution of the operation, and report on operative and oncologic outcomes.
We present the following article in accordance with the Narrative Review reporting checklist (available at http://dx.doi.org/10.21037/aoe-20-12).
Surgical technique: minimally invasive McKeown esophagectomy
Thoracic component
Following induction of general anesthesia, the patient is intubated with a single-lumen endotracheal tube. Flexible bronchoscopy is performed to rule out invasion of the airway, followed by flexible endoscopy to assess the extent of disease in the esophagus. The single-lumen endotracheal tube is then replaced with a left-sided double-lumen endotracheal tube. The operation begins with the patient in the left lateral decubitus position, with slight rotation anteriorly. Thoracoscopic ports are placed as described by Pennathur et al. (9). There are two ports for the primary surgeon posteriorly and two for the assistant anteriorly (or vice versa, depending on surgeon preference), along with one port for a 5-mm 45-degree camera. Carbon dioxide insufflation to 8 mmHg and/or a diaphragm retraction stitch is used to help improve visualization in the thoracic sulcus.
The esophagus is mobilized from the hiatus to the thoracic inlet using a vessel-sealing device. The authors prefer the LigaSure Maryland (Medtronic). The azygous vein is divided with a linear Endo GIA stapler (Medtronic). Lymph node stations 8 and 9 are removed en bloc with the esophagus, while a complete lymphadenectomy of the subcarinal and right paratracheal nodal packets is performed separately after esophageal mobilization. To prevent chylothorax, the thoracic duct proper is ligated if it is visualized. Care is taken to protect the recurrent laryngeal nerves as the dissection of the esophagus is continued into the thoracic inlet and neck. A circumferential Penrose drain is placed around the esophagus, secured with hemoclips, to facilitate retraction. This drain is ultimately left in place in the thoracic inlet to help identify the esophagus from the neck incision. A second Penrose drain is placed in the diaphragmatic sulcus and hiatus inferiorly to assist with retraction and easy identification of the esophagus during the abdominal phase of the operation. Once dissection is complete, a 28 French chest tube is placed through the most inferior port and positioned posteriorly and apically. An intercostal nerve block is then performed using liposomal bupivacaine, as no epidural is placed preoperatively.
Abdominal component
The patient is repositioned supine and secured with a foot board, arms tucked, and a shoulder roll is placed with the head directed toward the right to expose the left neck. A central port is placed below the falciform and above the umbilicus for the camera, followed by two ports for the primary surgeon in the left upper quadrant and two ports for the assistant in the right upper quadrant. This configuration is optimal if both a first and second assistant are available. An additional port is used at the xyphoid for the Nathanson liver retractor (Cook Medical).
Once the patient is placed in steep reverse Trendelenburg position, dissection begins at the lesser curve, and the gastrohepatic ligament is divided up to the hiatus (beware of a replaced left hepatic artery). Celiac axis lymphadenectomy is then performed, removing all lymph nodes along the hepatic artery and the left gastric artery. The left gastric artery is skeletonized and divided with the Endo GIA stapler, taking care to preserve the splenic artery.
The gastroepiploic arcade is then identified visually along the greater curve, and the lesser sac is entered through the gastrocolic ligament. The dissection is continued along the greater curve toward the left crus, ensuring that the short gastric artery branches are well cauterized. The dissection is then continued toward the duodenum, separating the stomach from the transverse mesocolon. The authors do not perform a gastric drainage procedure routinely. In addition, the authors do not perform a full Kocker maneuver, as fully releasing the peritoneal reflection along the gastroepiploic pedicle to the first portion of the duodenum is usually sufficient to allow the gastric conduit to reach the neck. Next, the phrenoesophageal ligament is divided, and the esophagus is circumferentially mobilized at the hiatus extending into the mediastinum. Continuity with the chest dissection is established by identifying the Penrose drain in the diaphragmatic sulcus. With full mobilization of the stomach complete, the gastric conduit is fashioned with serial firings of the linear Endo GIA stapler from the incisura to the tip of the fundus. A conduit diameter of 3–5 cm is preferred, and the conduit is completely detached from the specimen.
Last, a jejunostomy tube (J-tube) is placed. The patient is positioned in Trendelenburg position, and the omentum and transverse colon are retracted superiorly. The ligament of Treitz is identified, and a segment of jejunum 30–40 cm distal to the ligament is used to insert the J-tube. The Endo Stitch device (Medtronic) with a 2-0 Surgidac suture is used to place sutures in four quadrants to tack the jejunum to the abdominal wall. The J-tube is placed using the Seldinger technique, and an antitorsion stitch is placed once the tube is secured to the abdominal wall. The omentum and transverse colon are then returned to their normal anatomic position to prevent future herniation into the mediastinum.
Cervical component
A left neck incision along the anterior sternocleidomastoid muscle is made. The carotid sheath is retracted laterally, the thyroid is retracted medially, and the tracheoesophageal groove is identified. The recurrent laryngeal nerve may or may not be seen, but the dissection is limited to the plane immediately adjacent to the esophagus, and blunt techniques are used once the space is opened up. The dissection is continued toward the thoracic inlet, and continuity is established with the previous chest dissection, where the Penrose drain was retained. The specimen is pulled out carefully through the neck while the assistant feeds the distal end through the hiatus and mediastinum laparoscopically. The proximal esophagus is divided sharply with a knife, and the specimen is sent to pathology for frozen section analysis of the proximal and distal margins.
To facilitate bringing the conduit to the neck, a Foley catheter or chest tube is passed through the neck incision and posterior mediastinum and into the abdomen. The tip is secured to the gastric conduit using the Endo Stich device with a 2-0 Surgidac suture, and the conduit is brought up into the neck, again, with laparoscopic assistance in carefully feeding it through the hiatus in the correct orientation. The anastomosis is constructed with either a 25-mm or a 28-mm EEA stapler (Medtronic). A nasogastric tube is passed through the anastomosis and secured at 45 cm at the nares. A Jackson-Pratt drain is positioned beside the anastomosis, and the wounds are closed.
Minimally invasive McKeown esophagectomy: evolution and outcomes
The first descriptions of minimally invasive esophagectomy (MIE) were published more than 20 years ago. Similar to open approaches, MIE approaches were categorized broadly into transhiatal, transthoracic Ivor Lewis, and three-hole or McKeown. Transition from open to transhiatal MIE involved laparoscopy in the abdomen, often with a hand port to assist, followed by left neck incision and cervical anastomosis. In 1995, DePaula et al. published a case series of 12 patients undergoing transhiatal MIE in which only 1 conversion, due to an enlarged left lobe of the liver, was required (10). Similarly, in 1997 Swanstrom et al. reported a series of 9 patients undergoing transhiatal MIE in which no conversions were required and no anastomotic leaks were observed, although 1 patient did require an intrathoracic anastomosis due to a short gastric conduit (11).
The evolution of minimally invasive transthoracic esophagectomy took a more step-wise approach given the need to operate in two separate body cavities. The first report of a thoracoscopic esophagectomy was from Cuschieri et al. in 1992 (12). The largest initial experience, however, came from Luketich et al. in 2000, which included a combination of three surgical approaches: 60 patients underwent three-hole transthoracic McKeown MIE with laparoscopy, thoracoscopy, and cervical anastomosis; 9 patients underwent transhiatal MIE; and 8 patients underwent Ivor Lewis MIE with laparoscopic abdominal and minithoracotomy with intrathoracic anastomosis (13,14). There were only 4 conversions, due to adhesions, and no 30-day mortality. Rates of anastomotic leak and recurrent laryngeal nerve injury were 9.1% and 2.6%, respectively. These studies were able to establish the feasibility of esophagectomy using a minimally invasive approach, but numerous challenges were apparent. The operation is technically demanding and has a steep learning curve. Approximately 35 to 40 operations are required to achieve surgical proficiency in order to decrease surgical time, chest tube duration, and hospital length of stay (15). This surgical volume may be more likely to be achieved in a high-volume tertiary care center.
Subsequently, Luketich et al. went on to report a larger experience of transthoracic MIE, comprising 222 patients, all but 8 of whom underwent McKeown MIE (16). The conversion rate was 7.2%, all for nonemergent causes, with 5.4% requiring thoracotomy and 1.8% requiring laparotomy. Perioperative 30-day mortality was 1.4%, the anastomotic leak rate was 11.7%, and the gastric tip necrosis rate was 3.2%. Other pertinent complications included atrial fibrillation in 11.7%, pneumonia in 7.7%, and vocal cord paralysis in 3.6% of patients. Of note, a smaller diameter conduit, of 3–4 cm, was associated with a significantly higher leak rate (25.9% vs. 6.1%). Survival was comparable to that in a series of 342 patients who underwent open McKeown esophagectomy, although in the MIE cohort, stage II disease appeared to be associated with worse survival and stage III disease was associated with improved survival (17).
Outcomes: McKeown MIE versus Ivor Lewis MIE
One of the largest series of MIE compared McKeown MIE to Ivor Lewis MIE in 1,011 patients treated between 1996 and 2011 (18). McKeown MIE was performed in 48% of patients and Ivor Lewis MIE in 52%. The conversion rate was similar between the two approaches: 2.5% in McKeown MIE and 2.0% in Ivor Lewis MIE. There was no difference in postoperative length of stay or 30-day mortality (total mortality, 1.68%; Ivor Lewis MIE, 0.9%; McKeown MIE, 2.5%; P=0.083). Interestingly, although the overall anastomotic leak rate was not reported, the leak rate requiring surgery was 2.6% for McKeown MIE and 2.3% for Ivor Lewis MIE, with no statistical difference (P=0.439).
This study was influential given the noted differences in perioperative outcomes between the two approaches. Specifically, there was a higher incidence of vocal cord paralysis (3.7% vs. 0.5%; P<0.001) and acute respiratory distress syndrome (1.8% vs. 0.8%; P=0.026) in the McKeown MIE group. Given the changing patient demographics in North America, with decreased incidence of midesophageal tumors, intrathoracic anastomosis has become more prominent, as there may be reduced morbidity associated with neck dissection and vocal cord paralysis. To test this hypothesis directly, the Dutch ICAN trial was designed as a multicenter, randomized superiority trial with the goal of demonstrating a lower rate of anastomotic complications following intrathoracic esophagogastric anastomosis, compared with cervical esophagogastric anastomosis (19). This trial closed to accrual in late 2019, and results have yet to be reported. As such, other than the ICAN trial, many of the latest randomized controlled trials looking at outcomes after MIE do not include the three-field McKeown approach but rather only the two-field Ivor Lewis approach. Two completed trials, MIRO and MIOMIE, and one pending trial, ROMIO, compared open Ivor Lewis esophagectomy with hybrid Ivor Lewis esophagectomy using laparoscopy in the abdomen and thoracotomy in the chest (20-23).
Outcomes: comparison of open McKeown versus McKeown MIE
One of the first studies to look at the oncologic outcomes of McKeown MIE was by Law et al. (24). They performed a direct comparison of open McKeown esophagectomy and hybrid minimally invasive McKeown, where the hybrid approach used thoracoscopy in the chest and a laparotomy incision in the abdomen. Most patients had midesophageal cancer; of 85 patients, 18 underwent a hybrid approach, and 63 underwent a completely open approach. There were 4 conversions. There was 1 death—a patient who was converted to an open approach. The median number of lymph nodes harvested was 7 (range, 2–13) with thoracoscopy and 13 (range, 5–34) with thoracotomy, and 2-year survival was 62% after the hybrid approach versus 63% after the open approach. However, it is important to note that only 36 patients (44%) in the entire study population underwent curative-intent resection; the remainder received palliative operations. Another retrospective review compared patients who underwent open McKeown esophagectomy with those who underwent McKeown MIE (25). These patients all had early pathologic T1N0 carcinoma, and there was no difference in 5-year disease-specific or recurrence-free survival, with a median follow-up of 12 months. The overall 5-year survival in the entire group was 84.3%.
A meta-analysis of 1,212 patients from 16 case-control studies showed no difference in survival between open esophagectomy and MIE in all time intervals evaluated (30 days and 1, 2, 3, and 5 years), although surgical approaches included not only McKeown esophagectomy but also Ivor Lewis and transhiatal esophagectomy (26). MIE was associated with a higher lymph node yield than open esophagectomy, potentially secondary to the better visualization afforded by thoracoscopy, but the authors noted that the number of lymph nodes examined may also be related to the quality of pathological examination. A subsequent meta-analysis of 1,549 patients from 13 studies once again observed no compromise in oncologic outcomes with MIE, and this analysis excluded transhiatal approaches (27). There was no difference in 5-year survival and there was an improvement in 2-year survival with MIE. The results of these two meta-analyses should be viewed with caution, however, given the lack of level 1 evidence.
The best level evidence comparing open esophagectomy to MIE comes from the prospective TIME randomized controlled trial from Europe (28,29). The surgical approaches included both McKeown and Ivor Lewis esophagectomy, but there were at least twice the number of McKeown esophagectomy patients as Ivor Lewis patients, and transhiatal patients were excluded altogether. The R0 resection rate was 90.4% in the open group, compared with 98.2% in the MIE group, with no statistical difference. There was also no difference in the total number of lymph nodes retrieved between the two groups. After adjustment for stage, sex, and age, there was no difference in overall and disease-free survival at 3 years; however, the authors noted that the analysis by stage was underpowered. Overall survival was 41.2% in the open group versus 42.9% in the MIE group; disease-free survival was 37.3% in the open group versus 42.9% in the MIE group. The rate of recurrence was 62.5% in the open group versus 49.2% in the MIE group. The surgical conversion rate was 14%. There was no difference in the anastomotic leak rate, although the rate of vocal cord paralysis was higher in the open esophagectomy group (14% vs. 2%; P=0.012).
Of note, the primary endpoints of the study were pulmonary function and rate of pulmonary complications, and the results showed that, in the first 2 weeks of recovery, the open group had a pneumonia rate of 29%, compared with only 9% in the MIE group [relative risk, 0.30 (95% CI, 0.12–0.76); P=0.005]. Previous studies have shown that posterolateral thoracotomy reduces chest wall compliance, and hybrid McKeown esophagectomy has been shown to better preserve pulmonary function 3 months postoperative, compared with an open approach (30,31). Specifically, there were improvements in FEV1, vital capacity, and performance status. However, the best level of evidence comparing open McKeown esophagectomy with McKeown MIE may come from a randomized controlled trial underway in China, where there is still a relatively high incidence of midesophageal squamous cell cancers (32).
Robotic McKeown esophagectomy
The first report of robot-assisted transhiatal esophagectomy was in a case report in 2006, and this was soon followed by a case series of McKeown MIE in 2007 (33,34). There were 14 patients in total, with transition to robotic MIE performed in a step-wise fashion. The first patient underwent robot-assisted thoracoscopy for the chest portion and laparotomy for the abdominal portion. The next 3 patients underwent robot-assisted thoracoscopy and conventional laparoscopy, and the last 8 underwent robot-assisted thoracoscopy and laparoscopy. There were 2 anastomotic leaks and 1 case of bilateral vocal cord paralysis requiring tracheostomy. There was also 1 death, on postoperative day 3, from pneumonia and respiratory failure.
Thereafter, Sarkaria et al. published a series of robot-assisted McKeown and Ivor Lewis esophagectomy in 21 patients (35). Conversion to an open approach occurred in 24% of patients, but an additional 24% required conversion to either nonrobotic laparoscopy or thoracoscopy. The most common reason for conversion was inadequate visualization of the greater curve anatomy and the arterial arcade. There was no 30-day mortality, but 1 death occurred on postoperative day 70 from respiratory failure and anastomotic leak.
Outcomes: robotic compared with open McKeown esophagectomy
Larger series of robot-assisted esophagectomies are now available (Table 1). A randomized controlled trial from the Netherlands, the ROBOT study, compared open with robotic McKeown esophagectomy (38,40). There was no difference in R0 resection rates or the number of lymph nodes harvested. In addition, there were no differences in overall and disease-free survival. The operative time was longer for robotic than for open procedures (349 vs. 296 minutes; P<0.001), and the only statistically significant difference in perioperative outcomes was a lower rate of atrial fibrillation in the robotic group (22% vs. 46%; P=0.01).
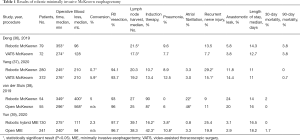
Full table
A retrospective series comparing robotic with open McKeown or Ivor Lewis esophagectomy analyzed 130 patients who underwent a hybrid robotic operation with conventional laparoscopy in the abdomen and robot-assisted thoracoscopy in the chest, with 241 patients undergoing an open operation (39). Once again, there was no difference in the R0 resection rate, with similar lymph node harvest. The open group had a higher proportion of patients undergoing induction therapy (42.3% vs. 16.2%; P=0.001); however, this did not appear to affect survival, as there was no difference in 3-year overall or disease-free survival. The robotic group had a lower rate of postoperative pneumonia than the open group (3.8% vs. 10.8%; P=0.035).
Outcomes: robotic MIE compared with McKeown MIE
Deng et al. performed a propensity score-matched analysis of 151 patients, comparing robotic with McKeown MIE (36). Robotic esophagectomy had a higher lymph node yield than MIE, and the authors concluded that the robot may have the advantage of more-extended lymphadenectomy, but no survival data were presented. A series of 652 patients from Yang et al. similarly compared robotic with open McKeown MIE in a propensity score-matched analysis (37). With respect to lymphadenectomy, there was no overall difference, but the robotic group had higher lymph node counts in the vicinity of the right recurrent laryngeal nerve, which also may explain the higher rate of vocal cord paralysis in the robotic group (29.2% vs. 15.1%; P<0.001). Importantly, overall and disease-free survival were not statistically different, and although the overall recurrence rate was not statistically significant, the rate of mediastinal lymph node recurrence was lower in the robotic group (2.0% vs. 5.3%; P=0.044).
Conclusions
McKeown, or three-hole, esophagectomy is the preferred operation for resection of midesophageal malignancies. Evolution from an open approach to a minimally invasive approach has resulted in a decrease in the perioperative morbidity associated with three-field dissection while not compromising oncologic outcomes. Minimally invasive McKeown esophagectomy represents a meaningful advancement in the surgical management of esophageal cancer, and this has been substantiated by the latest TIME randomized controlled trial. The results of an ongoing randomized trial directly comparing open with minimally invasive McKeown esophagectomy are eagerly anticipated. Moreover, robotic approaches to esophagectomy have proven to be safe and feasible and add another option to the surgeon’s armamentarium in the management of esophageal malignancies.
Acknowledgments
Funding: NIH/NCI Cancer Center Support Grant P30 CA008748.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Christopher R. Morse and Uma M. Sachdeva) for the series “Minimally Invasive Esophagectomy” published in Annals of Esophagus. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at http://dx.doi.org/10.21037/aoe-20-12
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/aoe-20-12). The series “Minimally Invasive Esophagectomy” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Torek F. The first successful resection of the thoracic portion of the esophagus for carcinoma. JAMA 1913;60:1533. [Crossref]
- Turner GG. Excision of thoracic esophagus for carcinoma with construction of extrathoracic gullet. Lancet 1933;2:1315. [Crossref]
- Adams WE, Phemister DB. Carcinoma of the lower thoracic esophagus. J Thoracic Surg 1938;7:621-32. [Crossref]
- Lewis I. The surgical treatment of carcinoma of the oesophagus with special reference to a new operation for growths of the middle third. Br J Surg 1946;34:18-31. [Crossref] [PubMed]
- McKeown KC. Total three-stage oesophagectomy for cancer of the oesophagus. Br J Surg 1976;63:259-62. [Crossref] [PubMed]
- Mallipeddi MK, Onaitis MW. The contemporary role of minimally invasive esophagectomy in esophageal cancer. Curr Oncol Rep 2014;16:374. [Crossref] [PubMed]
- Orringer MB, Sloan H. Esophagectomy without thoracotomy. J Thorac Cardiovasc Surg 1978;76:643-54. [Crossref] [PubMed]
- Dimick JB, Pronovost PJ, Heitmiller RF, et al. Intensive care unit physician staffing is associated with decreased length of stay, hospital cost, and complications after esophageal resection. Crit Care Med 2001;29:753-8. [Crossref] [PubMed]
- Pennathur A, Awais O, Luketich JD. Technique of minimally invasive Ivor Lewis esophagectomy. Ann Thorac Surg 2010;89:S2159-62. [Crossref] [PubMed]
- DePaula AL, Hashiba K, Ferreira EA, et al. Laparoscopic transhiatal esophagectomy with esophagogastroplasty. Surg Laparosc Endosc 1995;5:1-5. [PubMed]
- Swanstrom LL, Hansen P. Laparoscopic total esophagectomy. Arch Surg 1997;132:943-7; discussion 947-9. [Crossref] [PubMed]
- Cuschieri A, Shimi S, Banting S. Endoscopic oesophagectomy through a right thoracoscopic approach. J R Coll Surg Edinb 1992;37:7-11. [PubMed]
- Luketich JD, Nguyen NT, Weigel T, et al. Minimally invasive approach to esophagectomy. JSLS 1998;2:243-7. [PubMed]
- Luketich JD, Schauer PR, Christie NA, et al. Minimally invasive esophagectomy. Ann Thorac Surg 2000;70:906-11; discussion 911-2. [Crossref] [PubMed]
- Tapias LF, Morse CR. Minimally invasive Ivor Lewis esophagectomy: description of a learning curve. J Am Coll Surg 2014;218:1130-40. [Crossref] [PubMed]
- Luketich JD, Alvelo-Rivera M, Buenaventura PO, et al. Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 2003;238:486-94; discussion 494-5. [Crossref] [PubMed]
- Swanson SJ, Batirel HF, Bueno R, et al. Transthoracic esophagectomy with radical mediastinal and abdominal lymph node dissection and cervical esophagogastrostomy for esophageal carcinoma. Ann Thorac Surg 2001;72:1918-24; discussion 1924-5. [Crossref] [PubMed]
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [Crossref] [PubMed]
- van Workum F, Bouwense SA, Luyer MD, et al. Intrathoracic versus Cervical ANastomosis after minimally invasive esophagectomy for esophageal cancer: study protocol of the ICAN randomized controlled trial. Trials 2016;17:505. [Crossref] [PubMed]
- Mariette C, Markar SR, Dabakuyo-Yonli TS, et al. Hybrid Minimally Invasive Esophagectomy for Esophageal Cancer. N Engl J Med 2019;380:152-62. [Crossref] [PubMed]
- Paireder M, Asari R, Kristo I, et al. Morbidity in open versus minimally invasive hybrid esophagectomy (MIOMIE): Long-term results of a randomized controlled clinical study. Eur Surg 2018;50:249-55. [Crossref] [PubMed]
- Metcalfe C, Avery K, Berrisford R, et al. Comparing open and minimally invasive surgical procedures for oesophagectomy in the treatment of cancer: the ROMIO (Randomised Oesophagectomy: Minimally Invasive or Open) feasibility study and pilot trial. Health Technol Assess 2016;20:1-68. [Crossref] [PubMed]
- Brierley RC, Gaunt D, Metcalfe C, et al. Laparoscopically assisted versus open oesophagectomy for patients with oesophageal cancer-the Randomised Oesophagectomy: Minimally Invasive or Open (ROMIO) study: protocol for a randomised controlled trial (RCT). BMJ Open 2019;9:e030907 [PubMed]
- Law S, Fok M, Chu KM, et al. Thoracoscopic esophagectomy for esophageal cancer. Surgery 1997;122:8-14. [Crossref] [PubMed]
- Nafteux P, Moons J, Coosemans W, et al. Minimally invasive oesophagectomy: a valuable alternative to open oesophagectomy for the treatment of early oesophageal and gastro-oesophageal junction carcinoma. Eur J Cardiothorac Surg 2011;40:1455-63; discussion 1463-4. [Crossref] [PubMed]
- Dantoc M, Cox MR, Eslick GD. Evidence to support the use of minimally invasive esophagectomy for esophageal cancer: a meta-analysis. Arch Surg 2012;147:768-76. [Crossref] [PubMed]
- Guo W, Ma X, Yang S, et al. Combined thoracoscopic-laparoscopic esophagectomy versus open esophagectomy: a meta-analysis of outcomes. Surg Endosc 2016;30:3873-81. [Crossref] [PubMed]
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [Crossref] [PubMed]
- Straatman J, van der Wielen N, Cuesta MA, et al. Minimally Invasive Versus Open Esophageal Resection: Three-year Follow-up of the Previously Reported Randomized Controlled Trial: the TIME Trial. Ann Surg 2017;266:232-6. [Crossref] [PubMed]
- Peters RM, Wellons HA Jr, Htwe TM. Total compliance and work of breathing after thoracotomy. J Thorac Cardiovasc Surg 1969;57:348-55. [Crossref] [PubMed]
- Taguchi S, Osugi H, Higashino M, et al. Comparison of three-field esophagectomy for esophageal cancer incorporating open or thoracoscopic thoracotomy. Surg Endosc 2003;17:1445-50. [Crossref] [PubMed]
- Mu J, Gao S, Mao Y, et al. Open three-stage transthoracic oesophagectomy versus minimally invasive thoraco-laparoscopic oesophagectomy for oesophageal cancer: protocol for a multicentre prospective, open and parallel, randomised controlled trial. BMJ Open 2015;5:e008328 [Crossref] [PubMed]
- Gutt CN, Bintintan VV, Koninger J, et al. Robotic-assisted transhiatal esophagectomy. Langenbecks Arch Surg 2006;391:428-34. [Crossref] [PubMed]
- Kernstine KH, DeArmond DT, Shamoun DM, et al. The first series of completely robotic esophagectomies with three-field lymphadenectomy: initial experience. Surg Endosc 2007;21:2285-92. [Crossref] [PubMed]
- Sarkaria IS, Rizk NP, Finley DJ, et al. Combined thoracoscopic and laparoscopic robotic-assisted minimally invasive esophagectomy using a four-arm platform: experience, technique and cautions during early procedure development. Eur J Cardiothorac Surg 2013;43:e107-15. [Crossref] [PubMed]
- Deng HY, Luo J, Li SX, et al. Does robot-assisted minimally invasive esophagectomy really have the advantage of lymphadenectomy over video-assisted minimally invasive esophagectomy in treating esophageal squamous cell carcinoma? A propensity score-matched analysis based on short-term outcomes. Dis Esophagus 2019;32:doy110 [Crossref] [PubMed]
- Yang Y, Zhang X, Li B, et al. Short- and mid-term outcomes of robotic versus thoraco-laparoscopic McKeown esophagectomy for squamous cell esophageal cancer: a propensity score-matched study. Dis Esophagus 2020;33:doz080 [Crossref] [PubMed]
- van der Sluis PC, van der Horst S, May AM, et al. Robot-assisted Minimally Invasive Thoracolaparoscopic Esophagectomy Versus Open Transthoracic Esophagectomy for Resectable Esophageal Cancer A Randomized Controlled Trial. Ann Surg 2019;269:621-30. [Crossref] [PubMed]
- Yun JK, Chong BK, Kim HJ, et al. Comparative outcomes of robot-assisted minimally invasive versus open esophagectomy in patients with esophageal squamous cell carcinoma: a propensity score-weighted analysis. Dis Esophagus 2020;33:doz071 [Crossref] [PubMed]
- van der Sluis PC, Ruurda JP, van der Horst S, et al. Robot-assisted minimally invasive thoraco-laparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer, a randomized controlled trial (ROBOT trial). Trials 2012;13:230. [Crossref] [PubMed]
Cite this article as: Choi JJ, Sihag S. Minimally invasive McKeown esophagectomy: a narrative review of current operative and oncologic outcomes. Ann Esophagus 2021;4:16.


